Chronic Pelvic Pain Care Deserts
Medical deserts are defined by Branzac as areas where population healthcare needs are unmet partially or totally due to lack of adequate access or improper quality of healthcare services. Causes include insufficient human resources in health or facilities, long waiting times, disproportionately high costs of services or other socio-cultural barriers1. This month is Pelvic Pain Awareness Month and an opportunity to advocate for patients who are unable to find appropriate care for chronic pelvic pain.
The most recognized medical desert in the field of Obstetrics and Gynecology are maternal care deserts, defined as any county without a hospital or birth center that provides obstetric care and obstetric providers2. However, management of chronic pelvic pain (CPP) in rural areas is also a significant challenge. One reason for this is the lack of a clear definition for what qualifies as a Pelvic Pain Center. An AI inquiry characterized the key features of a Pelvic Pain Center:
- Comprehensive diagnosis: Advanced imaging, lab tests, and specialized evaluations to identify underlying causes.
- Multidisciplinary treatment: Offers a combination of medication, physical therapy, minimally invasive procedures, nerve blocks, and psychological support.
- Personalized care plans: Tailored treatments based on individual patient needs.
- Education and support: Guidance on lifestyle modifications, coping strategies, and mental health support.
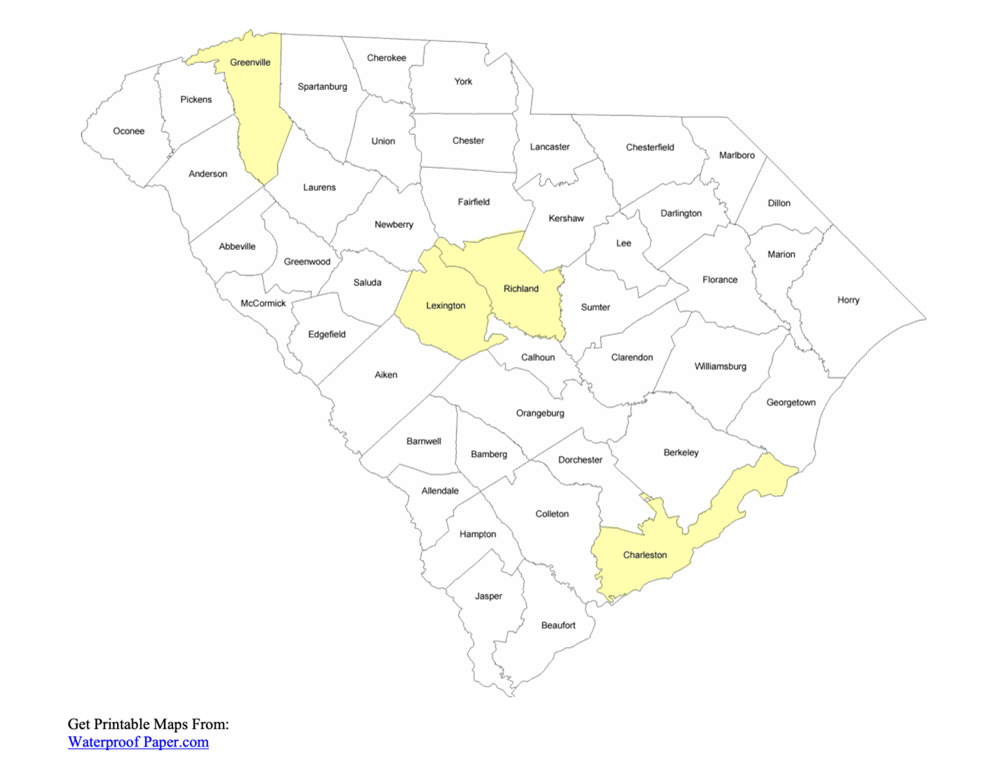
In South Carolina, a recent online search was done by a University of South Carolina medical student regarding the availability of specialized centers to diagnose and treat chronic pelvic pain4. This search revealed a total of 48 self-designated pelvic pain centers. Thirty-six of these centers were located in the counties that include the four primary urban centers of South Carolina, and just 32% of the population. Therefore, there are 39 out 46 counties with no reported pelvic pain centers.
 On a further analysis of the self-identified Pelvic Pain Centers services related to diagnosis and management, it was discovered that the majority provided only physical therapy and a variety of complementary treatment options. The second, most common medical services provided under this category were anesthesia and orthopedic interventional based management.
On a further analysis of the self-identified Pelvic Pain Centers services related to diagnosis and management, it was discovered that the majority provided only physical therapy and a variety of complementary treatment options. The second, most common medical services provided under this category were anesthesia and orthopedic interventional based management.
Only one center offered a broader approach that included a gynecologist, urogynecologist, physical therapy, and interventional anesthesia. There is limited information regarding psychological, gastroenterology or ortho-gyn involvement of these centers. Additionally, access to these centers based on insurance was not evaluated.
The lack of a standardized definition of a pelvic pain center, the added complexity of the multidisciplinary approach of CPP, and limited ability to access the available resources, especially in rural areas, creates an access gap for the quality pillar of providing the right service at the right time for the right reason.
A patient in a rural area, especially with remoteness or transportation concerns, that is looking for CPP care faces multiple challenges and confusion determining the best place to be treated.
In addition, health care providers in rural areas, often with reduced resources, are facing many challenges. They are not only required to provide care for the patients with CPP but also to establish an adequate referral system to specialized centers.
Experienced providers, with support from medical societies that embrace CPP care as one of their fundamental educational pillars, should further support this underserved patient population.
References
- Brînzac, Monica G., et al. “Defining medical deserts—an international consensus-building exercise.”European journal of public health 5 (2023): 785-788.
- https://www.marchofdimes.org/peristats/data?top=23
- https://chatgpt.com/c/67ed2a31-8850-800d-91a7-4beb233fc007
- Mary Hunter Hyche, “Healthcare Deserts of Chronic Pelvic Pain Management Centers in Women Leading to Undertreatment”, Poster Presentation, Discover USC 2025, Columbia SC, April 25, 2025.






