Spotlight On: Robotics

 This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Robotics Special Interest Group (SIG) led by Chair, Thiers Soares, MD, Dr.h.c.
This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Robotics Special Interest Group (SIG) led by Chair, Thiers Soares, MD, Dr.h.c.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
SIG Recommended SurgeryU Video #1:
Deep Infiltrating Endometriosis Affecting Ileoanal Anastomosis (J-Pouch): Surgical Approach
Kelsey A. Stewart, MD, Diana Encalada, MD, Zaraq Khan, MD, Tatnai Burnett, MD, Scott Kelley, MD, and Adela G. Cope, MD
This case involves deep infiltrating endometriosis (DIE) affecting a J-pouch, a surgically constructed ileoanal anastomosis typically performed after colectomy for conditions like ulcerative colitis. The overlap of DIE with altered colorectal anatomy is highly uncommon and requires tailored surgical strategy.
SIG Recommended SurgeryU Video #2:
Trachelectomy with Excision of Endometriosis for Chronic Pelvic Pain
Perrin Downing, MD, Sara Post, MD, Christine Santayana, DO, and Meenal Misal, MD
This case addresses a challenging scenario: chronic pelvic pain after subtotal hysterectomy due to residual cervical and deep infiltrating endometriosis. It shows how traquelectomy can be a definitive step in selected patients, something not routinely encountered in standard practice.
JMIG Article Recommendation #1:
Robot-Assisted Laparoscopic Hysterectomy With Artificial Intelligence-Analyzed Imaging
Naoyuki Yoshiki, MD, PhD, Noriko Oshima, MD, PhD, and Naoyuki Miyasaka, MD, PhD
The article presents an innovative approach to minimally invasive gynecologic surgery by integrating artificial intelligence (AI) into robot-assisted laparoscopic hysterectomy (RALH). It describes how AI-analyzed imaging can enhance real-time surgical navigation by identifying and labeling critical anatomical structures such as ureters, bladder, and blood vessels during the procedure. This AI support system operates alongside the robotic platform, assisting the surgeon by providing visual cues, anatomical overlays, and predictive risk alerts, which are particularly valuable in complex cases with distorted anatomy or prior surgeries.
This article is highly recommended because it represents a significant advancement in surgical technology. It brings together the precision of robotics with the cognitive support of AI, paving the way for a new era of intelligent, data-supported surgery. For gynecologic surgeons, particularly those dealing with challenging hysterectomy cases, this approach promises not only to improve outcomes but also to reshape how we teach, learn, and execute minimally invasive procedures in the future.
JMIG Article Recommendation #2:
Operative Time for Minimally Invasive Sacrocolpopexy: Comparison of Conventional Laparoscopy Versus Robotic Platform
Stephanie Glass Clark, MD, MSc, Alexandra I. Melnyk, MD, MEd, Michael Bonidie, MD, Lauren Giugale, MD, and Megan S. Bradley, MD
This article explores one of the most debated aspects of minimally invasive pelvic floor surgery: the difference in operative time between conventional laparoscopic sacrocolpopexy (LSCP) and robot-assisted sacrocolpopexy (RSCP). Sacrocolpopexy is a gold-standard procedure for apical prolapse, and both minimally invasive approaches aim to offer reduced morbidity and faster recovery compared to open surgery. However, operative efficiency and cost-effectiveness remain key concerns.
The study compares intraoperative time metrics across the two techniques, including total operative time, docking time (for robotic cases), suturing time, and mesh placement duration. The findings confirm that robot-assisted sacrocolpopexy typically results in a longer total operative time—primarily due to additional setup (docking) and increased time for suturing. Despite this, robotic surgery may offer ergonomic benefits, improved instrument dexterity, and easier learning curves for complex intracorporeal suturing, especially among less experienced laparoscopic surgeons.
This paper is recommended because it presents a balanced and evidence-based comparison of two widely used approaches for pelvic organ prolapse repair. It provides valuable insight for both trainees and practicing surgeons when deciding on the most appropriate surgical platform, factoring in operative efficiency, patient safety, and institutional resources. It also reinforces the idea that technology choice should be tailored to surgical context, expertise, and patient needs—not driven solely by operative time metrics.
Pelvic Endometriosis With Sciatic, Pudendal and Obturator Nerve Involvement
Clinical History:
This patient was referred to my office with a primary complaint of endometriosis-related chronic pelvic pain. In 2021, at age 38, she underwent fertility evaluation due to concern about age-related decline. Laboratory testing showed low AMH, and she proceeded with elective oocyte cryopreservation, retrieving 8 oocytes. She is currently trying to conceive spontaneously for about 6 months.
Her pain symptoms have progressively worsened, including dysmenorrhea, left-sided gluteal and posterior thigh pain strongly associated with menstruation, and occasional dyspareunia, especially in the premenstrual period. She reports incomplete bladder emptying and rare episodes of urinary leakage with coughing. She also experiences chronic low back pain.
She is currently undergoing orthopedic physical therapy and acupuncture, and reports partial improvement with dietary changes. Her medication regimen includes omega-3 and coenzyme Q10. She has no known drug allergies. Past medical history includes dengue fever and hysteroscopic septoplasty. She is G0P0 and highly motivated to achieve pregnancy.
Clinical Examination:
On bimanual examination, a firm, nodular lesion was palpated in the left posterior cul-de-sac in the topography of the left uterosacral ligament, with lateral extension toward both left pelvic and vaginal wall. The patient had BMI of 27.9 (69 kg, 157 cm) and maintains a physically active lifestyle.
Imaging:
Pelvic-MRI: Involvement of the left uterosacral ligament, nodular lesion in the rectosigmoid (1.1 cm), and involvement of the lumbosacral trunk, pudendal, obturator and sciatic nerves.
Final Diagnosis:
Pelvic endometriosis with deep infiltration of the left uterosacral ligament, rectosigmoid colon, sciatic obturator and pudendal nerves.
Surgical Intervention:
Robotic approach was performed. Intraoperative findings confirmed extensive endometriotic implants involving the pelvic peritoneum, left ovary, bowel and left pelvic side wall (Figs 1 and 2). Parametrial assessment revealed deep left-sided infiltration extending to the pelvic wall, while the right parametrium was spared. On the left side, a nodule was compromising the ureter (Figs 3 and 4), the obturator nerve was infiltrated along two-thirds of its course (Fig 5), and there was superficial infiltration of the lumbosacral trunk and sciatic nerve. Pelvic excision of the endometriotic tissue, intestinal discoid resection and radical left parametrectomy were made (Fig 6). At the end of the procedure, we chose to use indocyanine green (ICG) intravenously to check the viability of the vascularization of the ureteral wall due to its extensive dissection (Fig 7).
Outcome and Follow-Up:
After the surgery the patient experienced significant relief from pelvic pain and from the left leg and gluteal pain as well. Since the patient wanted to get pregnant, we decided not to use any hormonal medication. Fortunately, 5 months after the surgery, the patient spontaneously became pregnant.
Discussion:
This case reflects a highly complex and extensive form of deep infiltrating endometriosis, with multi-organ and nerve involvement, requiring advanced surgical dissection. The robotic approach allowed for precision in managing critical structures and achieving maximal disease clearance with fertility preservation
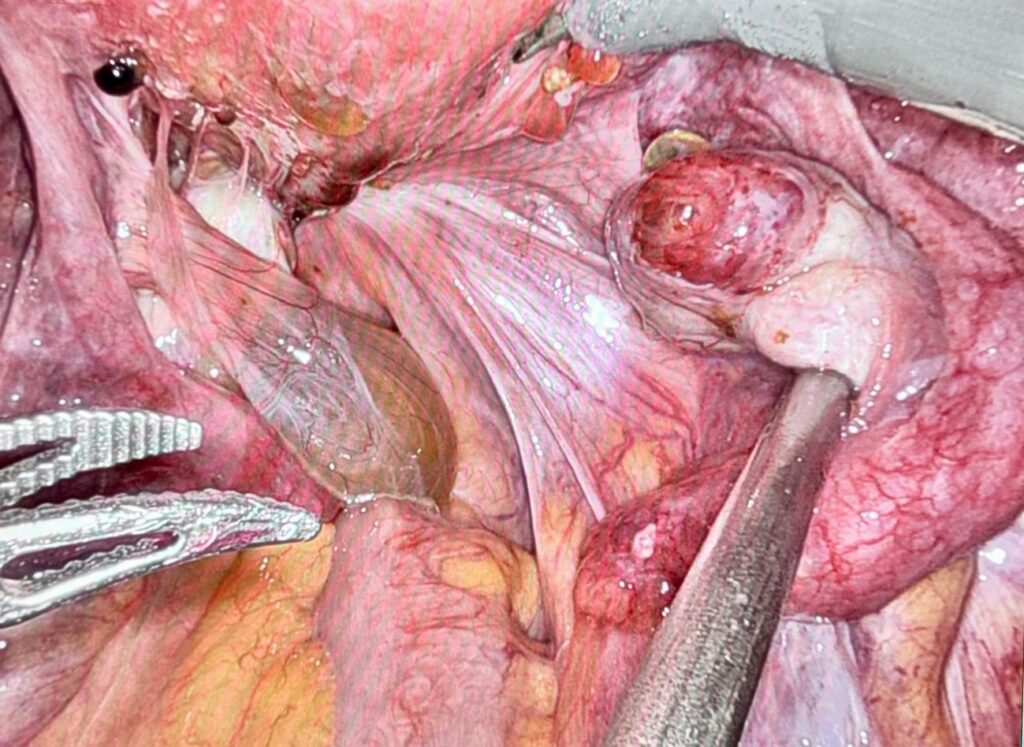 Figure 1: Initial View
Figure 1: Initial View
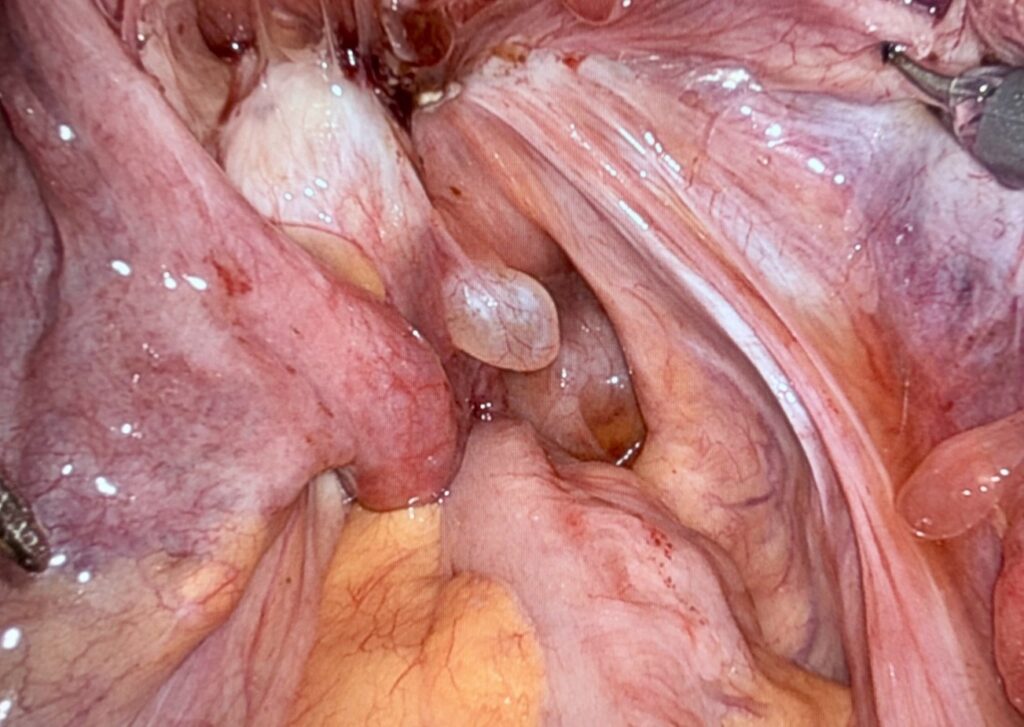 Figure 2: Initial View (Closer)
Figure 2: Initial View (Closer)
 Figure 3
Figure 3
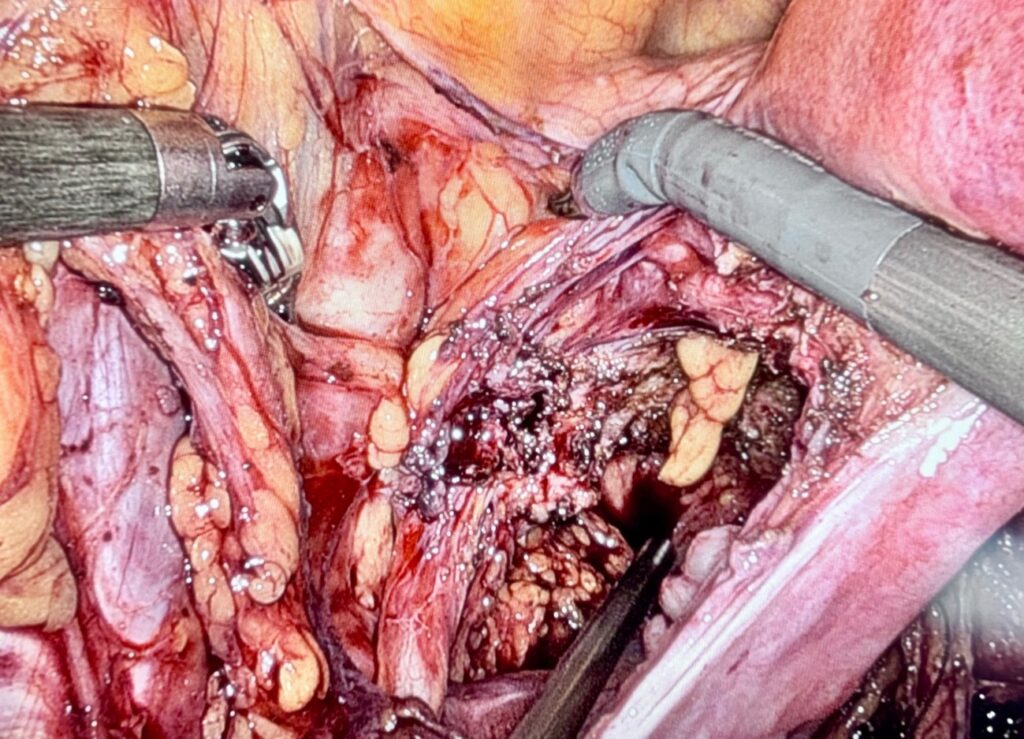 Figure 4
Figure 4
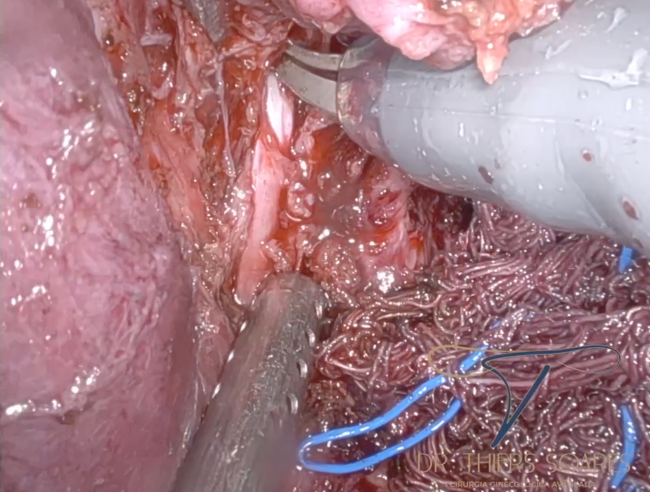 Figure 5: Obturator Nerve compromised by endometriosis nodule
Figure 5: Obturator Nerve compromised by endometriosis nodule
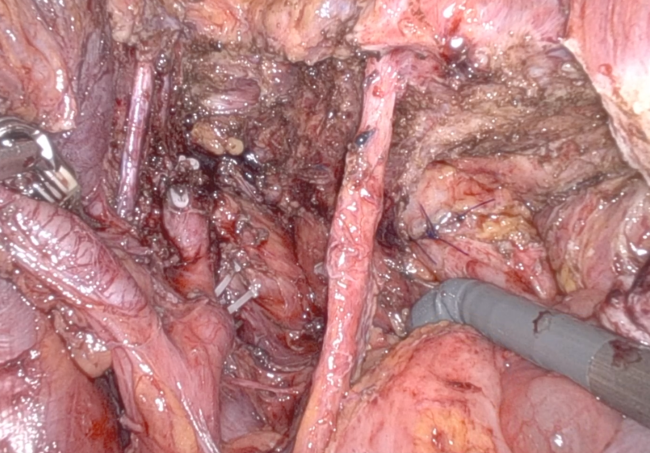 Figure 6: Final View
Figure 6: Final View
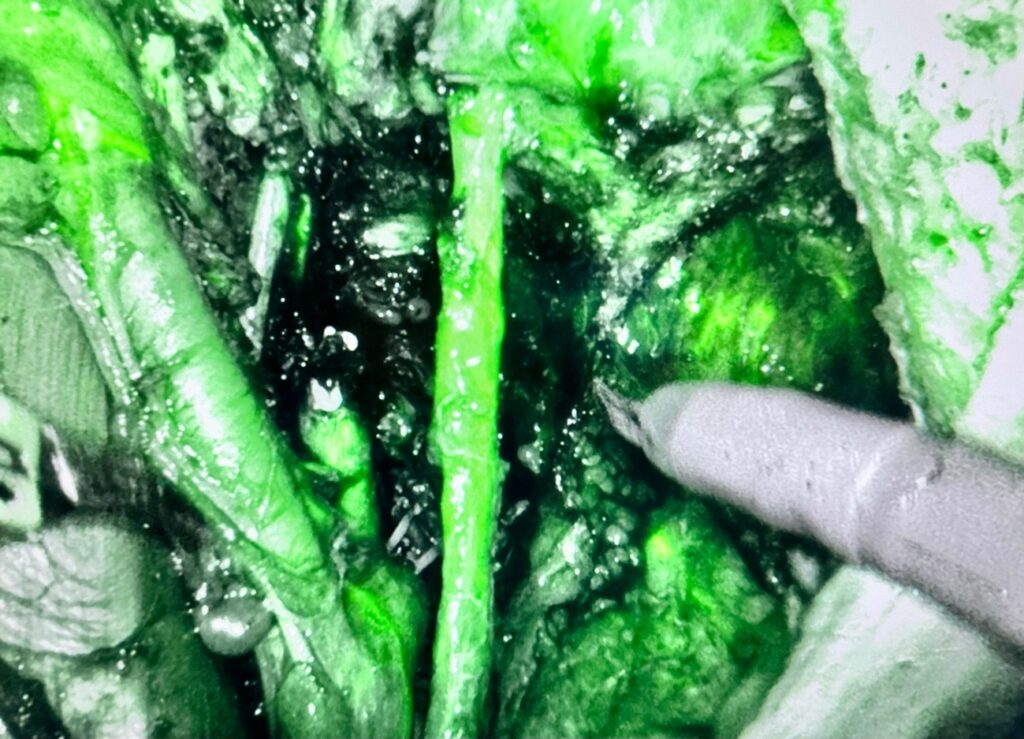 Figure 7: ICG View
Figure 7: ICG View
About the Author:
Thiers Soares, MD, Dr.h.c.

Dr. Soares is the Chair of the AAGL Robotics SIG and Gynecologic Surgeon at the State University of Rio de Janeiro Cardoso Fontes Federal Hospital in Rio de Janeiro, Brazil.
First Impressions: A Surgeon’s Perspective on the Intuitive DV5 Robot
In the evolving world of minimally invasive surgery, the Intuitive Da Vinci 5 is the latest leap forward, promising enhance precision, streamlined ergonomics, and an even more immersive surgical experience. Having performed a large number of cases on the Da Vinci Xi and now the DV5, I would like to share my initial thoughts and a practical comparison – from setup to counsel time – and how this next generation robot is shaping my expectations for the future of robotic assisted surgery.

Docking and Patient Cart: Familiar, Yet More Flexible
One of the first things I noticed was the robot’s refined footprint. The patient cart feels more compact and easier to maneuver around the OR table, a welcome change in tight operating rooms. Docking on the Xi is already relatively streamlined, but the DV5 refines this further. The set-up process seems to be more intuitive (pun intended) – docking feels smoother, with better articulation of the arms and fewer adjustments needed once the ports are placed.
Visualization: A Notable Step Up
Both platforms deliver excellent 3D high-definition vision, but the DV5 optics offer improved depth perception and crisper tissue contrast. This is particularly beneficial in severe endometriosis, where the difference between fibrotic tissue and vital structures can be subtle. Fluorescence imaging appears more stable and brighter on the DV5 compared to the Xi’s Firefly system.
Console Ergonomics: Designed for Surgeon Comfort
Ergonomics is where the DV5 stands out most distinctly. Sitting at the console, the difference is immediate. The redesigned surgeon console is noticeably more comfortable, with improved wrist rests and an adjustable viewing angle that reduces neck and shoulder strain during long cases. After performing back-to-back endometriosis resections and myomectomies on the DV5, I note less shoulder tension and less need to shift posture than I typically do with the Xi. Overtime, this ergonomic refinement could have a real impact on surgeon well-being, especially for high-volume surgeons.
Instrument Control and Responsiveness
In terms of end effector articulation and instrument variety, the platforms feel quite similar – both provide excellent dexterity for deep pelvic dissection. However, the DV5 introduces subtle but meaningful enhancements in instrument responsiveness and haptic-like feedback cues.
For example, during ureterolysis or parametrial dissection near critical vessels, the DV5’s improved tremor filtration and motion scaling deliver greater confidence in confined anatomy. The tactile awareness isn’t true haptics but rather a refined resistance feel, which I found somewhat helpful.
Smarter Workflow and Automation
Another stand out is the enhanced software integration. The DV5 introduces more customizable settings for different procedures and user preferences. It remembers instrument movements and positioning patterns, helping reduce repetitive tasks. This “smart memory” future could be a game changer in complex multi quadrant surgeries.
Instrument exchanges are faster too, with clearer alerts for instrument life and proactive maintenance notifications. Small improvements like these help the entire team stay ahead, keeping the flow of surgery smoother and minimizing downtime. Minutes may be shaved off of multi-instrument cases which can be an underrated but real benefit for high-complexity procedures with frequent tool swaps.
Learning Curve and Adaptation
For experienced Da Vinci Xi users, the learning curve feels minimal. The fundamentals remain the same, but the refinements in vision, dexterity, and ergonomics make the transition worthwhile. The console controls, arm docking principles, and port placements are highly similar, so experienced Xi surgeons should feel at home within just a few cases. The main difference is getting used to the console adjustments and new arm boom range, which, in my experience, did not require dedicated re-training.
Final Thoughts
Overall, my first impressions of the intuitive DV5 are very positive. It builds on the strengths of its predecessor while addressing some of the day-to-day frustrations that only become apparent after hundreds of hours at the console – improved visualization for subtle disease, more ergonomic comfort for lengthy deep pelvic cases, and smarter system feedback to enhance intraoperative flow.
For gynecologists who rely on the Xi, the DV5 is not a dramatic overhaul but rather a thoughtful evolution – refining what already works and smoothing out common pain points. As adoption spreads and more surgeons share their experiences, I am excited to see how these advancements will push the boundaries of what is possible in minimally invasive surgery – and how they will inspire the next wave of robotic innovation.
Conflict of Interest Disclosure: Consultant and Proctor for Intuitive but not paid for my thoughts in this article.
About the Author:
Erica Stockwell, DO, MBA

Dr. Stockwell is a member of the AAGL Robotics SIG and a Gynecologic Surgeon at AdventHealth in Celebration, Florida, USA.