Spotlight On: Pediatric and Adolescent Gynecology
 This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Pediatric and Adolescent Gynecology Special Interest Group (SIG) led by Chair, Stephanie M. Cizek, MD.
This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Pediatric and Adolescent Gynecology Special Interest Group (SIG) led by Chair, Stephanie M. Cizek, MD.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
SIG Recommended SurgeryU Video #1:
Modified Wharton-Sheares-George Vaginoplasty With OASIS Graft: An Outpatient Surgical Procedure for Neovagina Creation
Dana Elborno, MD, Julia Geynisman, MD, Sara Muttar, Elizabeth Yerkes, MD, and Julia Grabowski, MD
This video demonstrates neovaginal creation using a technique that avoids the need for either abdominal entry or tissue grafted from the patient’s own body. The video highlights a simplified technique to create the vaginal space, using a porcine acellular scaffold to line the vaginal space.
SIG Recommended SurgeryU Video #2:
Laparoscopic Excision of an Accessory Cavitated Uterine Mass (ACUM) in an Adolescent Patient
Olga Kciuk, MD, MSc, and Stephanie Cizek, MD
ACUM is a rare uterine anomaly that is often misdiagnosed. This video demonstrates laparoscopic excision of an ACUM, highlighting the anomalous anatomy, key points to consider for diagnosis and safe surgery, and the histologic findings that support a diagnosis of ACUM.
JMIG Article Recommendation #1:
Surgical Considerations in the Management of Adolescent Endometriosis – An Expert Commentary
Jessica Shim, MD, Ted Lee, MD, Cara R. King, DO, MS, Jon Einarsson, MD, MPH, Mark D. Hornstein, MD, Marc R. Laufer, MD
This article outlines distinct surgical considerations in the management of endometriosis in adolescents and highlights the benefit of early diagnosis of endometriosis in patients presenting with dysmenorrhea. Additionally, it provides a call to action for ongoing research in surgical outcomes in adolescents with endometriosis, as a paucity of data on this topic currently exists and management recommendations are strongly reliant on expert opinion.
JMIG Article Recommendation #2:
Ultrasound Findings of Adenomyosis in Adolescent: Type and Grade of the Disease
Caterina Exacoustos, MD, PhD, Francesco G. Martire, MD, Consuelo Russo, MD, Simona Martone, MD, Gabriele Centini, MD, PhD, Emilio Piccione, MD, PhD, and Errico Zupi, MD
This article reviews ultrasounds of older adolescents and demonstrates that findings of adenomyosis can be identified in this age group. Adenomyosis is often thought of as a progressive disease impacting myometrial tissue in adults, however, this article serves as a reminder that adenomyosis can be a factor impacting dysmenorrhea in adolescents as well.
Article Summary Provided By:
Allison Mayhew, MD, FACOG

Dr. Mayhew is a member of the AAGL PAG SIG and Director of Pediatric and Adolescent Gynecology at Children’s National Hospital in Washington, DC.
This is a strange and exciting time to be writing an update on Pediatric and Adolescent Gynecology (PAG). The landscape of PAG has changed, and, as MIGS providers will understand, our growth means we are an ever-greater force for advocacy and for shaping the future of gynecologic care and training. This is particularly important now, when so many of us are facing uncertainties in our research funding and in regulations of our care.
There are now over 200 PAG Focused Practice Designation exam-certified specialists in the USA and Canada, and there are 18 fellowship programs; these numbers increase every year. The North American Society for Pediatric and Adolescent Gynecology (NASPAG) membership is expanding both in numbers and geographic involvement, and our international colleagues at the World Congress of PAG will be joining us in San Francisco in April 2026 for a large, combined conference. We invite our MIGS colleague to join us at our NASPAG conferences and learn more about providing gynecologic care for our younger patients (and share your own knowledge!). https://www.naspag.org/acrm-future-and-past
PAG and MIGS specialists are both great collaborators. In PAG, gynecologic conditions in young patients often arise in the setting of other complex medical needs. From congenital anomalies and differences of sex development, to bleeding from hematologic disorders or iatrogenic bleeding in young cardiac patients, to fertility preservation before gonadotoxic treatments or gyn care after those treatments, we by necessity are experts in multidisciplinary care. MIGS specialists who collaborate in pain clinics or fibroid centers will recognize the extra effort that it takes for multidisciplinary coordination.
It’s not surprising then that we would collaborate with each other, and we are proud and grateful for our MIGS colleagues who are interested in strengthening these partnerships. AAGL now has a PAG spotlight month in February, a growing PAG SIG, and at the November 2024 AAGL conference there were multiple PAG abstracts and two PAG-focused postgraduate courses – with more to come next year! The conversations between our fields have most recently resulted in NASPAG endorsing an Endometriosis Care Quality Collaborative (soon to be published in JMIG) and increasing research and clinical opportunities are in the works.
PAG and MIGS represent an age spectrum of complex gynecologic care. Our growing pains and growing successes as subspecialties are similar, and we face overlapping advocacy, reimbursement, and research challenges. We look forward to our continued growth within AAGL and invite surgeons interested in working with young people to collaborate with our SIG to address the research gaps in our field.
About the Author:
Stephanie Cizek, MD

Dr. Cizek is Chair of the AAGL PAG SIG, a Clinical Associate Professor in Pediatric and Adolescent Gynecology, Medical Co-Director of the Differences of Sex Development Clinic, founder of Stanford’s Complex Colorectal-Urology-Gynecology Clinic, Pediatric Lead for Fertility Preservation, and the PAG Fellowship Director at the Stanford University School of Medicine in Stanford, California.
High Vaginal Septum in Obstructed Hemi Vagina and Ipsilateral Renal Anomaly (OHVIRA) Syndrome Managed With Pneumovaginal Surgery
Review:
Obstructed Hemivagina and Ipsilateral Renal Anomaly (OHVIRA) is defined by a Müllerian anomaly with unilateral obstructed hemivagina and associated renal anomaly (image 1).
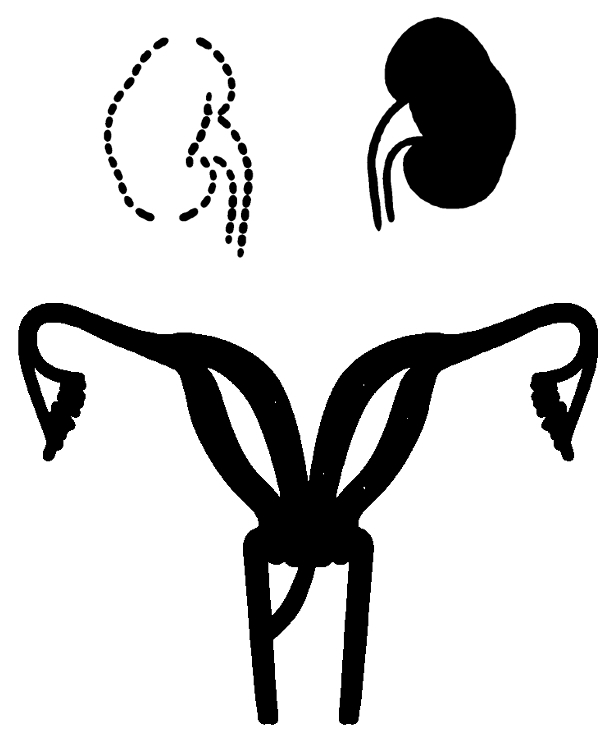
Image 1: Representation of OHVIRA
Patients typically present after menarche with pain due to hematocolpos on the affected side. Patients often undergo a staged procedure with placement of a transvaginal drain, or a single procedure to resect the obstructing vaginal septum. However, transvaginal resection of a high septum can be technically challenging, limited by instrument length and introital size in recently menarchal patients. Pneumovaginal surgery with the use of transanal platforms has been described for excision of longitudinal septae and eroded mesh. We present the first use of pneumovaginal surgery for management of a high obstructing septum.
Case Presentation:
An 11-year-old female with history of a solitary left kidney presented to the ER with severe dysmenorrhea. On imaging, she was found to have uterus didelphys with an obstructed right hemivagina (image 2).
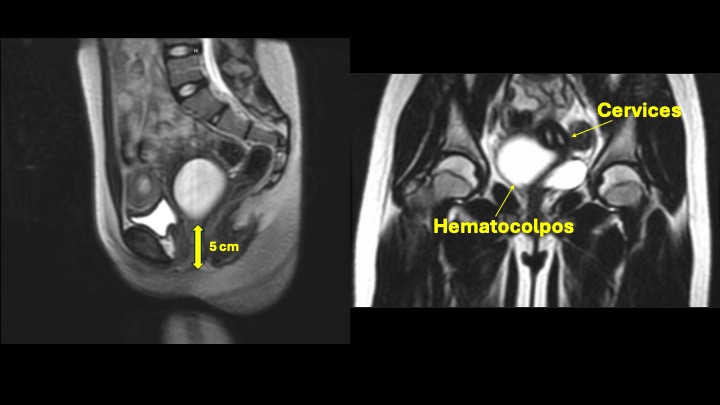
Image 2: MRI demonstrating obstructed right hemivagina, with septum >5cm from the introitus.
She was discharged from an outside hospital on an OCP taper and returned to the ER with abdominal pain after decreasing her dose. She was taken to the OR for examination under anesthesia and was found to have a high vaginal septum, with the inferior-most aspect 5 cm proximal to the introitus. Due to difficulty accessing the obstructed hemivagina, she underwent ultrasound-guided placement of a transvaginal 20 French Malecot drain (image 3). She was suppressed with norethindrone acetate.
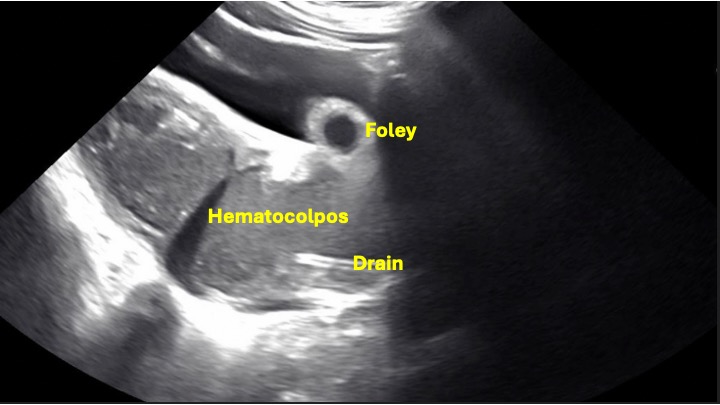 Image 3: Intraoperative ultrasound demonstrating placement of transvaginal drain.
Image 3: Intraoperative ultrasound demonstrating placement of transvaginal drain.
Given the distance of the obstruction from the introitus and difficulty with visualization, the decision was made to proceed with pneumovaginal resection of the septum 6 weeks after drain placement, to allow for inflammation to improve for optimal tissue healing, and to ensure excellent menstrual suppression. The GelPOINT Path Transanal Access Platform 4 cm access channel was placed within the introitus to provide atraumatic retraction (image 4).
 Image 4: The GelSeal Transanal Access Platform
Image 4: The GelSeal Transanal Access Platform
The GelSeal cap was attached to the access channel, and the vagina was insufflated to 8 mmHg using an insufflation stabilization bag. A 30-degree laparoscopic camera was introduced, and the vaginal septum and left cervix were visualized (image 5).
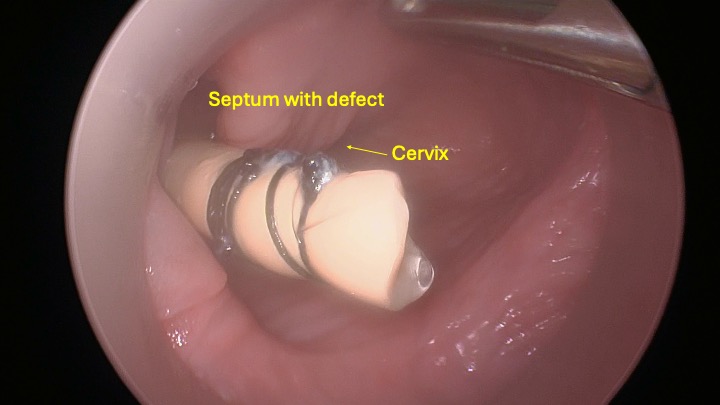
Image 5: Initial pneumovaginal appearance of the vaginal septum and left sided cervix.
The right cervix was visualized through the defect in the septum. An approximately 2 by 1.5 cm area of septum was excised, approximately 0.8 cm thick using the Harmonic scalpel and monopolar hook. Interrupted sutures of 3-0 polysorb were used to reapproximate the mucosa anteriorly. Posteriorly there was need for hemostasis, and the mucosa was reapproximated using 3-0 stratafix. Irrigation was performed and hemostasis was confirmed with both cervices visualized at the apex of the unified vagina (image 6).
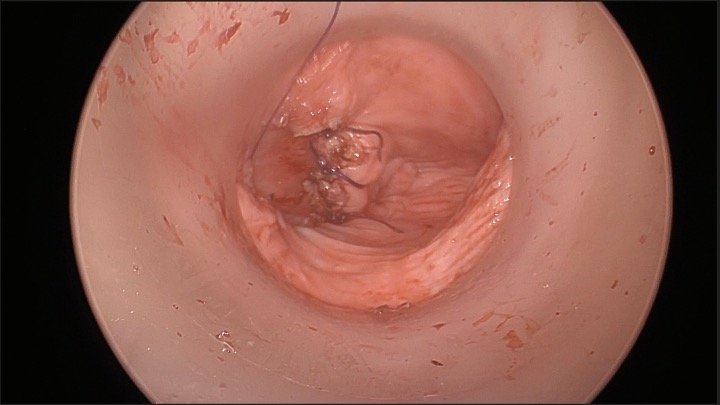 Image 6: Postoperative appearance with bilateral cervices visualized and minimal residual septum.
Image 6: Postoperative appearance with bilateral cervices visualized and minimal residual septum.
Digital exam confirmed palpation of two cervices with minimal residual septum, approximately 0.5 cm. Rectal exam ensured intact rectal mucosa. Lidocaine gel was placed intravaginally. The patient tolerated the procedure well and was discharged home after voiding.
Conclusion:
Pneumovaginal resection of an obstructing vaginal septum is a minimally invasive, feasible approach in a young patient with OHVIRA. Application of this surgical technique may result in improved visualization and has potential to result in more complete excision of the vaginal septum in challenging cases.
References:
- Billone, V., Amorim-Costa, C., Campos, S., Rabischong, B., Bourdel, N., Canis, M., & Botchorishvili, R. (2015). Laparoscopy-like operative vaginoscopy: a new approach to manage mesh erosions. J Minim Invasive Gynecol, 22(1), 10. https://doi.org/10.1016/j.jmig.2014.09.004
- Breech, L. L., & Laufer, M. R. (2009). Mullerian anomalies. Obstet Gynecol Clin North Am, 36(1), 47-68. https://doi.org/10.1016/j.ogc.2009.02.002
- Heredia, F., Donetch, G., Escalona, J., & Hinostroza, M. (2020). Single-Port/Pneumovagina Technique for Two Further Applications. J Minim Invasive Gynecol, 27(4), 807-808. https://doi.org/10.1016/j.jmig.2019.06.014
- Shabanov, S., Hurni, Y., Lopes, A., & Brossard, P. (2023). Pneumovaginal endoscopic surgery to vaginal septum resection: a case report and literature review. Gynecology and Pelvic Medicine, 6. https://gpm.amegroups.org/article/view/9158
- Smith, N. A., & Laufer, M. R. (2007). Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil Steril, 87(4), 918-922. https://doi.org/10.1016/j.fertnstert.2006.11.015
About the Authors:
Taryn Wassmer, MD
Krista Childress, MD
Lesley Breech, MD



Dr. Wassmer is a member of the AAGL PAG SIG and a second-year Fellow of Pediatric and Adolescent Gynecology in the Department of Pediatric Surgery at Cincinnati Children’s Hospital Medical Center in Cincinnati, Ohio.
Dr. Childress is a current member and former chair of the AAGL PAG SIG and an Associate Professor of Pediatric and Adolescent Gynecology in the Department of Pediatric Surgery at Cincinnati Children’s Hospital Medical Center in Cincinnati, Ohio.
Dr. Breech is a member of the AAGL PAG SIG and the Division Director of Pediatric and Adolescent Gynecology in the Department of Pediatric Surgery at Cincinnati Children’s Hospital Medical Center in Cincinnati, Ohio.

Intraoperative Laparoscopic Ultrasound
The use of intraoperative laparoscopic ultrasound for the resection of small benign ovarian tumors holds tremendous potential for optimizing ovarian-sparing techniques, especially in young patients. Ovarian-sparing surgery aims to remove pathological lesions while preserving as much functional ovarian tissue as possible, thereby maintaining hormonal and reproductive function. While often benign, adolescent ovarian tumors and cysts pose an increased risk of recurrence due to the patient’s age and extended reproductive lifespan. Additionally, these patients may be more likely to develop subsequent ovarian pathology requiring repeat surgical resection, compounding the risk of injury to baseline ovarian function.
One notable application of intraoperative laparoscopic ultrasound is in the localization of clinically significant masses, such as small mature teratomas or dermoids associated with NMDA receptor-positive antibodies. Dermoids are the most common type of germ cell tumor. In the pediatric and adolescent population, the recurrence rates are as high as 10%, though these tumors are typically benign. While asymptomatic or incidentally discovered lesions that are small may be monitored, patients with NMDA receptor-positive encephalitis, found to have a suspicious ovarian cyst/lesion require prompt surgical resection regardless of lesion size.
Laparoscopic ultrasound is available in various configurations and has long been used intraoperatively for lesion guidance in general surgery, including procedures involving the liver, gallbladder, and kidneys. The equipment consists of a probe and a scanner connected by a cable. The probes, typically less than 10 mm in diameter and 35–50 cm in length, can be utilized for ovarian evaluation through standard surgical port sites (10–12 mm) at the level of the umbilicus. The transducer is located at the tip of the shaft, with options for both linear and convex (curvilinear) arrays. A frequency range of 7–8 MHz allows for the clear visualization of even sub centimeter ovarian lesions.
Contact scanning on the surface of the ovary directly, as opposed to stand-off scanning—where the area of interest is immersed in a fluid medium such as saline—is sufficient for precise tumor localization. Contact scanning can also be performed in the supine position, through a laparoscopic trocar, in contrast to intraoperative ultrasound using transabdominal approach, which results in reduced image clarity with insufflation for laparoscopy or transvaginal and transrectal probes, which require the dorsal lithotomy position. A four-way laparoscopic transducer with a linear array provides additional flexibility for accessing difficult-to-reach areas, and an atraumatic instrument can be used to stabilize the ovary for strategic incision planning. The transducer head can be flexed left, right, upwards and downward with the use of a knob at the handle. Surgical resection can be performed with real-time ultrasound guidance to maximize ovarian tissue preservation. Additionally, post-resection ultrasound can confirm complete tumor removal.
Ovarian-sparing surgery is a critical approach in the management of small benign ovarian tumors, particularly in young patients for whom preserving ovarian function is a priority. Advances in ultrasound technology, including higher-resolution laparoscopic probes and robotic transducers, enhance tumor localization, facilitate precise resection, and ultimately improve surgical outcomes and long-term reproductive potential.
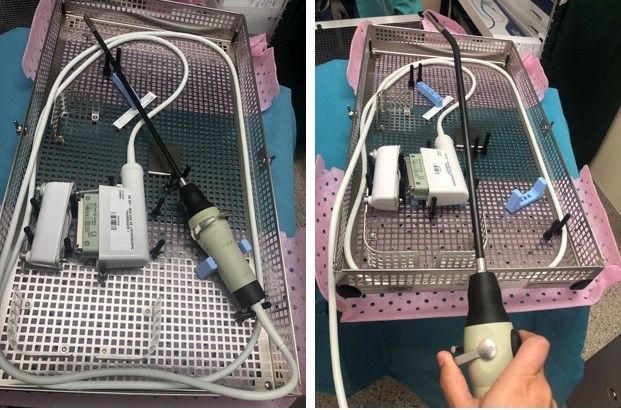 Image: Laparoscopic Ultrasound Probe
Image: Laparoscopic Ultrasound Probe
References:
- Jones BP, Rees R, Saso S, Stalder C, Smith JR, Yazbek J. Ultrasound-guided laparoscopic ovarian preserving surgery to treat anti-NMDA receptor encephalitis. BJOG. 2017 Jan;124(2):337-341. doi: 10.1111/1471-0528.14214. Epub 2016 Jul 17. PMID: 27425649.
- Kasaven LS, Galazis N, et al., Glob Libr Women’s Med. ISSN: 1756-2228; DOI 10.3843/GLOWM.419763
- Mascilini F, Quagliozzi L, Bolomini G, Scambia G, Testa AC, Fagotti A. Intraoperative ultrasound through laparoscopic probe in fertility-sparing surgery for borderline ovarian tumor recurrence. Ultrasound Obstet Gynecol. 2019 Aug;54(2):280-282. doi: 10.1002/uog.20138. PMID: 30288807.
About the Authors:
Georgina F. Amaral, MD, MSL, FACOG
Jennifer E. Dietrich, MD, MSc, FACOG


Dr. Amaral is a member of the AAGL PAG SIG, Assistant Professor in Pediatric and Adolescent Gynecology, Department of Obstetrics, Gynecology and Reproductive Sciences, Division of Advanced Minimally Invasive Gynecology (AMIG) and Assistant Professor Adjunct, Department of Pediatrics, Division of Adolescent Medicine at UTHealth Houston McGovern Medical School in Houston, Texas.
Dr. Dietrich is a member of the AAGL PAG SIG, Professor in the Department of Obstetrics and Gynecology and Department of Pediatrics, Chief of the Division and Fellowship Program Director of Pediatric and Adolescent Gynecology at Baylor College of Medicine at Texas Children’s Hospital, in Houston, Texas.