Spotlight On: Pelvic Pain

 This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Pelvic Pain Special Interest Group (SIG) led by Chair, Andrian Balica, MD.
This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Pelvic Pain Special Interest Group (SIG) led by Chair, Andrian Balica, MD.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
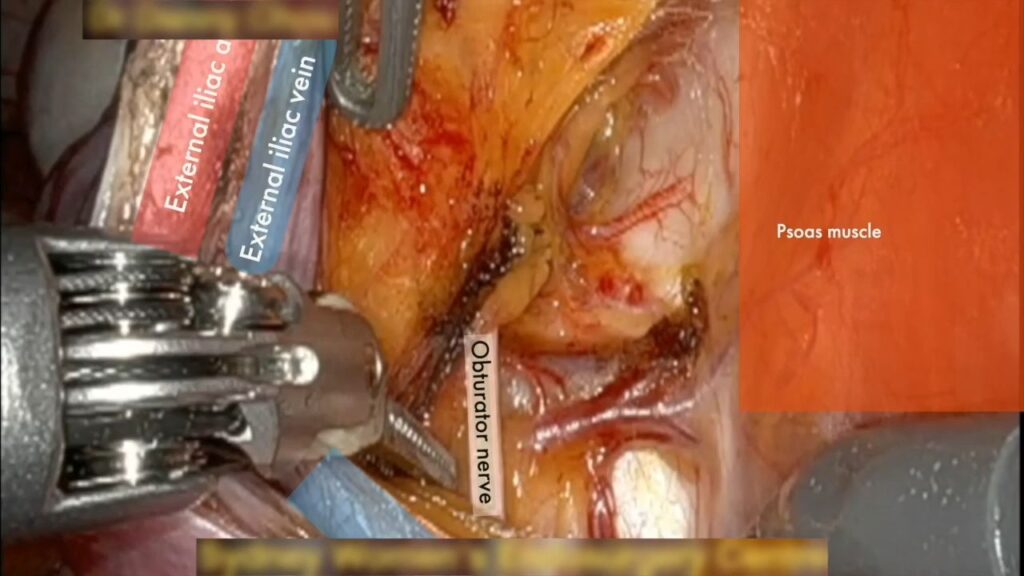
SIG Recommended SurgeryU Video #1:
Neuropelveology – Sciatic Nerve Decompression
By Mikhail Sarofim, BMed MD, MS
This video presents an excellent intraperitoneal dissection of the sciatic nerve, showcasing practical neuroanatomical surgical exposure.
Pelvic pain is a common presentation for gynecologists, however an important condition that is not well documented when discussing pelvic pain is caused by dilated and aberrant branches of the internal iliac vessels. This vascular dilation causes pressure and entrapment on the sacral plexus nerves including the sciatic nerve. Patients will present with sciatic back and lower limb neuralgia, and/or refractory urinary/anorectal dysfunction. We will present a video of a 26-year-old woman who suffered from debilitating right sided lower limb and pelvic pain, as well as bowel dysfunction. Design: This is a video case report presentation with labelled anatomy. Our patient presented to us after many unremarkable ultrasounds, CTs, a colonoscopy and MRIs before eventually presenting for review at our unit. Her symptoms began post-partum; a pregnancy that was complicated by severe pelvic girdle pain requiring a wheelchair and a subsequent retained placenta. Post-partum she had severe right-sided hip and posterior thigh pain (S1,S2,S3), posterior/lateral calf pain (L4,L5,S1) and heel pain (S1,S2). At its worst she was bed-bound. She mobilized with difficulty with a walking aid and was taking regular opioids. Interventions: The patient underwent robotic decompression of her sciatic nerve plexus secondary to vascular entrapment Measurements and Main Results: Intra-operatively findings there were multiple aberrant vessels compressing the lumbo-sacral trunk, sciatic nerve and pudendal nerve. The patient immediately reported her pain had resolved in recovery and was mobilizing without aids on day 1 post-operatively. She is no longer on any opioids for pain relief and is completely pain-free. Conclusion: This case highlights a less common cause of pelvic pain. Vascular entrapment of the sacral plexus should be considered when a patient presents with sciatic/bowel/bladder symptoms without any detectable pathology/precipitating factors. Finally, although effective, it does require experience with laparoscopy/robotic techniques and pelvic nerve anatomy and specialist referral is recommended.
SIG Recommended SurgeryU Video #2:
Pelvic Nerve Blocks
By Joanna Gao, MD and Mark Paul Lachiewicz, MD, MPH
This video demonstrates office-based nerve block procedures that are straightforward to perform by gynecologists and offer achievable diagnostic and therapeutic outcomes.
To demonstrate nerve block techniques for the obturator nerve, pudendal nerve, and uterine nerves (paracervical block). Design: Procedural video. Setting: Academic medical center. Patients or Participants: Patients with chronic pelvic pain. Interventions: This video demonstrates how to perform obturator, pudendal, and paracervical nerve blocks. This video highlights the techniques of these pelvic floor nerve blocks and includes general management and follow-up principles for these patients. Measurements and Main Results: Pain scores, on a scale of 0-10, are measured prior to and after nerve blocks to gauge response. Conclusion: Determining the source of chronic pelvic pain can be difficult for gynecologists. Nerve blocks can be an effective strategy to help evaluate and possibly treat pelvic pain. Pelvic floor nerve blocks can delineate whether or not pain is originating from the pelvic floor, uterus, or other source. Nerve blocks can also potentially be therapeutic in instances of nerve entrapment, muscle spasms, neuralgia, or myofascial pain. These instructional videos on administering pelvic floor nerve blocks can help gynecologists provide an additional source of therapy for their patients.
JMIG Article Recommendation #1:
Key Anatomical Concepts, Landmarks, and Proposed Terminology for Nerve-Sparing Gynecologic Surgery: A Narrative Review
Anna Kobylianskii, MD, Peter Thiel, MD, Meghan McGrattan, MD, Mary F. Barbe, PhD, and Nucelio Lemos, MD, PhD
This article is recommended because it underscores the significance of adopting standardized anatomical terminology to promote clearer understanding within the gynecology discipline and to facilitate more effective interdisciplinary collaboration. Furthermore, it proposes a refined nomenclature intended to enhance communication in the context of nerve-sparing surgical procedures in gynecology.
JMIG Article Recommendation #2:
Keep Your Landmarks Close, and the Hypogastric Nerve Closer: An Approach to Nerve-Sparing Endometriosis Surgery
Andrew Zakhari, MD, Mohamed Mabrouk, MD, PhD, Diego Raimondo, MD, M. Jonathon Solnik, MD, Ally Murji, MD, MPH, Nucelio Lemos, MD, PhD
This video article is recommended as it is a well-narrated and animated surgical presentation that enhances the understanding of anatomy and landmarks crucial for nerve-sparing surgery in gynecology.
Technology Updates in Chronic Pelvic Floor Pain: The Evidence Behind New Devices and Treatments
Chronic pelvic pain affects 15 – 29% of patients presenting for gynecologic care and can be extremely challenging to treat. There is a broad differential diagnosis including endometriosis, adenomyosis, pelvic floor tension myalgia, painful bladder syndrome, genitourinary syndrome of menopause, irritable bowel syndrome, pudendal neuralgia, vulvodynia, chronic vaginitis, fibromyalgia, and central sensitization, among others. Patients may present with multiple pain syndromes, and the chronic nature of this condition can be disheartening.
In today’s world, patients often turn to friends, family, and social media for guidance on how to manage medical conditions, especially if they do not experience improvements from conventional medical treatment. Furthermore, pelvic pain is challenging for clinicians and access to therapy is widely variable based on the resources available in different areas.
This has led to the development of new devices and procedures promising quick results with minimal downtime, coupled with eye-catching marketing and testimonials. Recently, a patient of mine showed me an advertisement on Instagram for a local medical spa offering vaginal red-light rejuvenation for pelvic pain. Due to her busy work and home schedule, she couldn’t attend pelvic floor physical therapy sessions and wanted an easy solution to resolve her pain. This interaction sparked my interest on the medical evidence behind these treatments.
An article published in 2024 showed that experts in management of high-tone pelvic floor dysfunction recommend pelvic floor physical therapy (PFPT) as the first-line gold standard management, followed by vaginal suppositories, trigger point injections, and pelvic floor Botox injections. [1] These recommendations are supported by numerous studies demonstrating symptomatic improvement, improved quality of life, and responses to validated questionnaires. Most of these treatments are covered by standard medical insurance, with the exception of Botox which is off-label for pelvic floor myalgia and often requires prior authorization and/or appeals for coverage, despite increasing evidence supporting its use.
Vaginal dilators, pelvic wands, and biofeedback are also beneficial by allowing patients to target trigger points and perform myofascial release. [2] Dilators serially and slowly stretch vaginal epithelium and pelvic floor muscles, which helps with painful intercourse. There are many brands and types of dilators and wands; some with thermal, cold, and vibrating capabilities which can aid with muscle relaxation. Popular brands include Intimate Rose, SoulSource, and Bodyotics. The Milli expanding dilator is a single dilator which inflates to the desired size once inserted vaginally. The Kiwi and the OhNut customizable penetration device (both available from The Pelvic People) relax muscles and limit depth of penetration. Goals of use are similar: massage, relax, and release tense muscles to reduce pain. These devices are easy to use, affordable, and can be used in conjunction with PFPT; although there is no high-quality data comparing brands, material, or standard clinical protocols on use. [3]
There are several other treatments that aim to improve symptoms with less work. First, let’s discuss SoLa Pelvic Therapy, a photobiomodulation device which uses transvaginal application of a near-infrared laser to the levator ani muscles. The device delivers therapeutic irradiance to the muscles and bladder. [4] A similar device was studied in a 2022 randomized controlled trial in Brazil where patients with myofascial pain were treated with vaginal stretching plus 10 sessions of photobiomodulation versus vaginal stretching and sham laser. Results show that both groups had improved sexual pain outcomes with no statistically significant differences. [5]
The vFit device (Joylux) uses high-powered ultraviolet-free red lights, thermal energy, sonic vibration, and photonic gel with hyaluronic acid to stimulate, encourage blood flow, and moisturize vaginal tissue. [6] It is used by the patient for approximately 10 minutes per day. Published work demonstrates improved Female Sexual Function Index (FSFI) scores and up to 83% patient satisfaction, as well as improvements in urinary incontinence and vaginal lubrication. [7, 8]
There are even more treatments available when the search is expanded to vaginal rejuvenation, but beyond the scope of this article. The point is that pelvic floor pain is debilitating, with impacts to daily life, ability to exercise, and personal relationships. Evidence-based treatments to address pelvic floor pain are time-intensive and limited based on availability of resources. There are many promising new technologies aimed at improving pelvic floor health. However, clinicians and researchers should evaluate these therapies for safety, efficacy, and long-term impacts. Furthermore, many of the published studies that support these devices used concurrent pelvic floor physical therapy or stretching, making it difficult to evaluate whether the device or the physical therapy resulted in the outcomes. Our priorities should be to inform patients of risks, benefits, and expectations, especially when treatments are costly and not covered by insurance. We should support industries with promising technology in order to improve our armamentarium and toolkit, while also evaluating these devices with high-quality longitudinal research.
References:
- Torosis, Michele et al. “A Treatment Algorithm for High-Tone Pelvic Floor Dysfunction.” Obstetrics and gynecology 143,4 (2024): 595-602. doi:10.1097/AOG.0000000000005536
- Jokar, Farnaz et al. “Effectiveness of Biofeedback with Dilator Therapy for Sexual Function in Women with Primary Vaginismus: Randomized Controlled Trial Study.” International urogynecology journal 36,3 (2025): 557-565. doi:10.1007/s00192-024-06011-y
- Liu, Marisa et al. “Vaginal Dilators: Issues and Answers.” Sexual medicine reviews 9,2 (2021): 212-220. doi:10.1016/j.sxmr.2019.11.005
- Zipper, Ralph, and Brian Pryor. “Evaluation of a novel deep tissue transvaginal near-infrared laser and applicator in an ovine model.” Lasers in medical science 37,1 (2022): 639-643. doi:10.1007/s10103-021-03315-z
- Frederice, Claudia Pignatti et al. “Effect of Vaginal Stretching and Photobiomodulation Therapy on Sexual Function in Women With Pelvic Floor Myofascial Pain – A Randomized Clinical Trial.” The journal of sexual medicine 19,1 (2022): 98-105. doi:10.1016/j.jsxm.2021.10.008
- Website: https://joylux.com/products/vfit-gold?tw_source=google&tw_adid=&tw_campaign=21704468128&gad_source=1&gbraid=0AAAAADMefpexOIJDj6oHuv20SJhBFuDuH&gclid=EAIaIQobChMIp_zbgLyhjAMV-qtaBR2OvRWQEAAYASAAEgKQVvD_BwE
- de la Torre S, Miller LE. Multimodal vaginal toning for bladder symptoms and quality of life in stress urinary incontinence. Int Urogynecol J. 2017;28(8):1201-1207. doi:10.1007/s00192-016-3248-5
- Alexiades, Macrene. “Device-based treatment for vaginal wellness.” Seminars in cutaneous medicine and surgery 37,4 (2018): 226-232. doi:10.12788/j.sder.2018.052
- Website: https://pelvicrehabilitation.com/services/pelvic-pain-specialists/prm-protocol/
About the Author:
Aakriti R. Carrubba, MD

Dr. Carrubba is a member of the AAGL Pelvic Pain SIG and Consultant of Minimally Invasive Gynecologic Surgery, Assistant Professor of Obstetrics and Gynecology and Associate Program Director of the Fellowship of Minimally Invasive Gynecologic Surgery at the Mayo Clinic in Jacksonville, Florida.