Spotlight On: Fibroids

 This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Fibroids Special Interest Group (SIG) led by Chair, Scott Chudnoff, MD, MSc, CPE, FACOG.
This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Fibroids Special Interest Group (SIG) led by Chair, Scott Chudnoff, MD, MSc, CPE, FACOG.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
SIG Recommended SurgeryU Video #1:
Enhancing Myomectomies With 3D Uterine Modeling
Erica Lynn Stockwell, DO
SIG Recommended SurgeryU Video #2:
Periurethral Leiomyoma: An Uncommon Finding
Veronica D. Galaviz, MD, Anthony D. Nguyen, MD, Peter L. Sticco, MD, and Keith T. Downing, MD
JMIG Article Recommendation #1:
Radiofrequency Ablation for the Treatment of Uterine Fibroids: A Systematic Review and Meta Analysis by the AAGL Practice Committee
Innie Chen, MD, MPH, Jay M. Berman, MD, Ethan M. Balk, MD, MPH, Ian J. Saldanha, MBBS, MPH, PhD, Emilie Kowalczewski, MSc, Johnny Yi, MD, Salena Zanotti, MD, Mariam Al Hilli, MD, Kimberly A. Kho, MD, MPH
A comprehensive meta-analysis examining RFA outcomes—fibroid size reduction, symptom relief, and safety—with data aggregated from over 30 studies.
JMIG Article Recommendation #2:
Conservative Treatment of Uterine Myomas: A Network Meta Analysis of Randomized Controlled Studies
Mattia Dominoni, MD, PhD, Barbara Gardella, MD, Andrea Gritti, MD, Marianna Francesca Pasquali, MD, Arsenio Spinillo, MD
This network meta-analysis of RCTs compares myomectomy, UAE, HIFU, and RFA, assessing reintervention rates, complications, and quality of life outcomes.
A Call to Action: Harnessing AI to Transform Uterine Tumor Diagnosis
Uterine fibroids are among the most common gynecologic conditions, affecting millions of women worldwide. Yet, despite their prevalence, our ability to distinguish benign leiomyomas from rare but aggressive uterine sarcomas remains limited. For many patients, this diagnostic uncertainty leads to invasive interventions that might otherwise be avoidable. As complex benign gynecologic surgeons, we are uniquely positioned to change this paradigm—and the time to act is now.
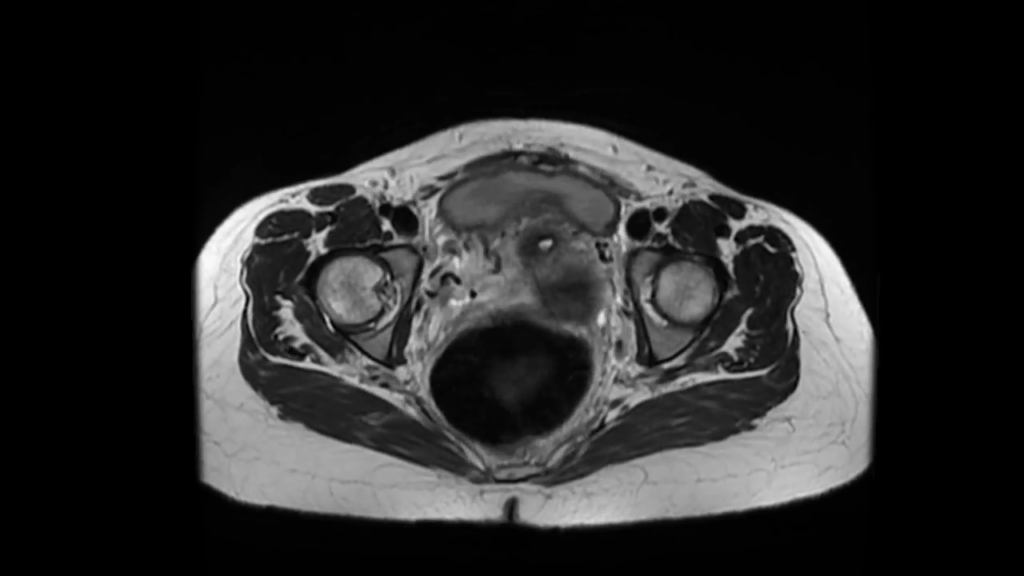
Traditional imaging techniques, while invaluable, are largely qualitative and dependent on human interpretation. Radiologists and surgeons rely on visual cues and subjective assessments that often cannot definitively rule out malignancy. Emerging technologies—artificial intelligence (AI), radiomics, and machine learning—offer a powerful opportunity to overcome these limitations. By extracting thousands of quantitative features from standard imaging modalities such as ultrasound or MRI, radiomics can reveal hidden patterns linked to tumor biology. When combined with machine learning algorithms, these patterns have the potential to differentiate benign from malignant uterine tumors with unprecedented precision [1,2].
Efforts are already underway to develop predictive models that integrate radiomic signatures, clinical metadata, and histopathologic outcomes. These approaches could transform preoperative risk stratification, reduce unnecessary surgeries, and guide truly personalized treatment strategies [3,4]. For patients, this means not only improved safety but also greater confidence in their care decisions.
Imagine a future where, during a routine ultrasound, an AI-powered tool analyzes the imaging data in real time and generates a malignancy risk score. Cases with atypical features could be flagged for further evaluation, while clearly benign fibroids could be safely monitored—empowering both patients and clinicians with actionable insights. This vision is no longer theoretical. Pilot studies across oncology have already demonstrated the power of radiomics in distinguishing benign from malignant lesions, and gynecology should not be left behind [5].
However, advancing this technology requires our active engagement. As surgeons, we must partner with radiologists, physicists, and engineers to build high-quality, well-annotated datasets. We must advocate for research funding that prioritizes the intersection of AI and women’s health, an area that remains underrepresented in biomedical innovation. Equally important, we must ensure that these tools are developed with equity in mind, addressing the disproportionate burden of fibroids and misdiagnosis in Black women.
As a complex benign gynecologic surgeon and clinical investigator, I have been privileged to contribute to this evolving landscape. In a recent pilot study, we applied radiomics and quantitative multiparametric MRI to predict fibroid growth trajectories. Using principal component analysis, we developed a promising model that identified fibroids with elevated growth rates—supporting the potential for tailored, fibroid-specific management strategies once validated in larger cohorts [6]. These tools offer complementary data to decode tumor behavior beyond what is visible on conventional imaging. While efforts are ongoing to secure funding and validate predictive models across diverse populations, the momentum is clear. Surgeons must not only understand these technologies—we must help shape their development, champion clinical integration, and ensure they are applied ethically and equitably. The future of uterine tumor diagnosis demands our leadership.
References
- Stewart EA, Laughlin-Tommaso SK, Catherino WH, Lalitkumar S, Gupta D, Vollenhoven B. Uterine fibroids. Nat Rev Dis Primers. 2016;2:16043. Published 2016 Jun 23. doi:10.1038/nrdp.2016.43
- Gillies RJ, Kinahan PE, Hricak H. Radiomics: Images Are More than Pictures, They Are Data. Radiology. 2016;278(2):563-577. doi:10.1148/radiol.2015151169
- Jacob H, Dybvik JA, Ytre-Hauge S, et al. An MRI-Based Radiomic Prognostic Index Predicts Poor Outcome and Specific Genetic Alterations in Endometrial Cancer. J Clin Med. 2021;10(3):538. Published 2021 Feb 2. doi:10.3390/jcm10030538
- Lu D, Yan Y, Jiang M, et al. Predictive value of radiomics-based machine learning for the disease-free survival in breast cancer: a systematic review and meta-analysis. Front Oncol. 2023;13:1173090. Published 2023 Aug 16. doi:10.3389/fonc.2023.1173090
- Santoro M, Zybin V, Coada CA, et al. Machine Learning Applied to Pre-Operative Computed-Tomography-Based Radiomic Features Can Accurately Differentiate Uterine Leiomyoma from Leiomyosarcoma: A Pilot Study. Cancers (Basel). 2024;16(8):1570. Published 2024 Apr 19. doi:10.3390/cancers16081570
- Drukker K, Medved M, Harmath CB, Giger ML, Madueke-Laveaux OS. Radiomics and quantitative multi-parametric MRI for predicting uterine fibroid growth. J Med Imaging (Bellingham). 2024;11(5):054501
About the Author:
Obianuju Sandra Madueke-Laveaux, MD, MPH

Dr. Madueke-Laveaux is a member of the AAGL Fibroids SIG and Associate Professor of Obstetrics & Gynecology in the Division of Minimally Invasive Gynecologic Surgery, Director at the Center for Advanced Treatment and Research (CATeR) of Uterine Fibroids, and Gynecologic Surgery Liaison at the Bloodless Medicine Program at the University of Chicago in Chicago, Illinois.
.