Spotlight On: Advanced Gynecologic Ultrasound & Imaging

 This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Advanced Gynecologic Ultrasound & Imaging Special Interest Group (SIG) led by Chair, Sophia N. Palmer, MD.
This month we cast a spotlight on articles, SurgeryU videos, and Journal of Minimally Invasive Gynecology (JMIG) article recommendations from the AAGL Advanced Gynecologic Ultrasound & Imaging Special Interest Group (SIG) led by Chair, Sophia N. Palmer, MD.
Access to SurgeryU and JMIG are two of the many benefits included in AAGL membership. The SurgeryU library features high-definition surgical videos by experts from around the world. JMIG presents cutting-edge, peer-reviewed research, clinical opinions, and case report articles by the brightest minds in gynecologic surgery.
SurgeryU video recommendations by our SIGs are available for public access for a limited time. The links to JMIG article recommendations are accessible by AAGL members only. For full access to SurgeryU, JMIG, CME programming, and member-only discounts on meetings, join AAGL today!
SIG Recommended SurgeryU Video #1:
NEW to SurgeryU! Accessory Cavitated Uterine Malformation (ACUM) Ultrasound Diagnosis
Alessandra Di Giovanni, MD
SIG Recommended SurgeryU Videos: Surgical Repair of Isthmocele
Globally, cesarean delivery is a common surgical procedure and is the most common surgery performed in the United States.
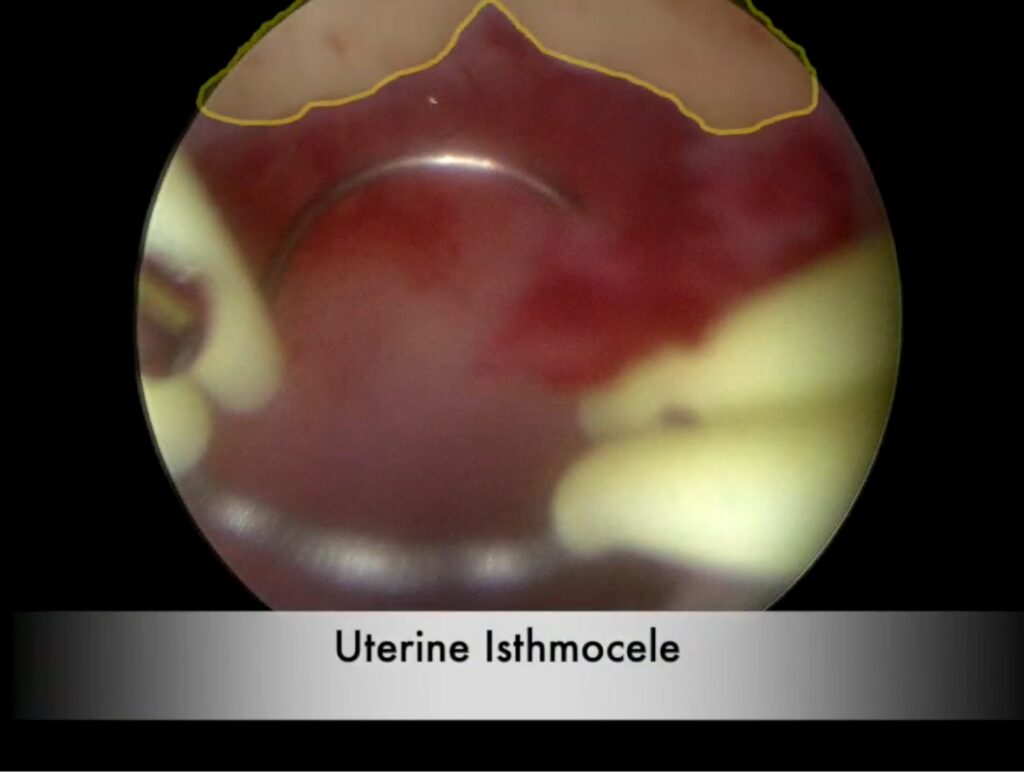
Cesarean scar defect, or isthmocele, can cause symptoms such as abnormal uterine bleeding, dysmenorrhea, infertility, etc. Diagnosis and characterization of the defect can easily be performed using ultrasound prior to surgical intervention.
These two articles demonstrated two minimally invasive approaches to the repair of isthmoceles: the first using conventional laparoscopy and illumination using a hysteroscope for intraoperative identification and the second video utilizes robotic-assisted laparoscopic repair with incorporation of Firefly technology for isthmocele detection.
SIG Recommended SurgeryU Video #2:
Surgical Management of Uterine Isthmoceles
Veronica Fox, MD, Olga Fajardo, MD, Elizabeth Cook, MD, Ted L. Anderson, MD, PHD, Howard Curlin, MD
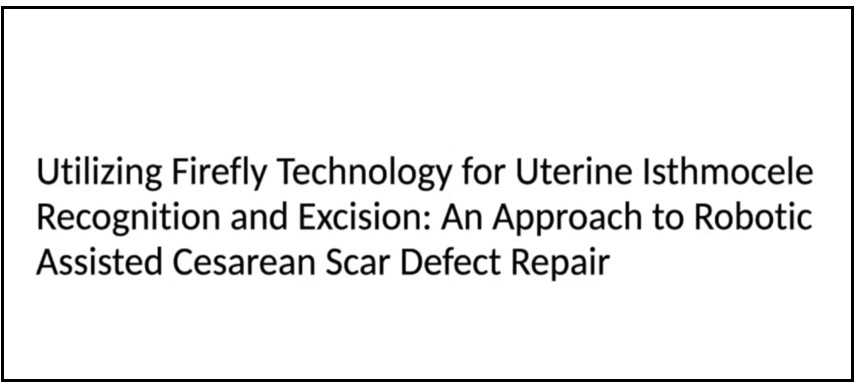
SIG Recommended SurgeryU Video #3:
Utilizing Firefly Technology for Uterine Isthmocele Recognition and Excision: An Approach to Robotic Assisted Cesarean Scar Defect Repair
Melanie Evans, MD, Patrick Michael Weix, MD, PhD, Charles Herrin, MD, Orhan Bukulmez, MD
JMIG Article Recommendation #1:
We recommend this important article that presents an international and intersociety consensus statement regarding the use of noninvasive imaging techniques, particularly transvaginal ultrasound and magnetic resonance imaging, in the preoperative diagnosis of endometriosis.
There are also many classification and scoring systems for endometriosis; the article addresses the use of TVS and MRI in the pre-operative classification of endometriosis using these systems.
JMIG Article Recommendation #2:
High-Intensity Focused Ultrasound Treatment for Rectal Endometriosis: A New Tool in Minimally Invasive Approaches?
A. Mazard, MD, C-A. Philip, MD, PhD, P. Rousset, MD, PhD
Ultrasound is most commonly known for its diagnostic use, but high intensity focused ultrasound (HIFU) is a treatment modality that uses high intensity, and highly focused, sound waves to modify or destroy target tissue. It has been used and investigated as a treatment modality for certain solid, malignant as well as in benign tumors including fibroids.
Bowel resection in the treatment of endometriosis is a surgical treatment option depending on lesion characteristics. Although curative, it can be associated with complications. This article presents the case of a woman treated with HIFU for rectal endometriosis.
A prospective multicenter study with 60 patients, evaluating the safety of the procedure was previously published by Dubernard, et al in 2024.
Decidualized Endometriomas Mimicking Ovarian Malignancy in Pregnancy
In 2013, a 23-year-old G2P1 at 18 weeks, 3 days gestation presented for a fetal anatomic survey. She had recently arrived from Guatemala, had a prior uncomplicated vaginal delivery, negative past medical and surgical history, and no prior ultrasounds.
Ultrasound revealed bilateral ovarian cysts but no fetal anomalies. Transvaginal ultrasound showed a 61 × 39 × 34 mm unilocular solid cyst in the left ovary with moderate color flow, and a similar cyst on the right. The lesions had features concerning for malignancy. The patient was referred to gynecologic oncology and underwent vertical laparotomy two weeks later. Frozen section of the left ovarian cyst revealed decidualized endometriosis, and surgery was terminated. She subsequently had an uncomplicated full-term pregnancy.
This case led us to conduct a retrospective study to identify features that could differentiate decidualized endometriomas from ovarian malignancy. We found that if the solid component remained stable in size, it was most likely a decidualized endometrioma. Decidualization is a progesterone-driven process, though for unknown reasons, most endometriomas do not undergo this change. Subsequent studies have shown that cysts with smooth-walled papillations and low-level or ground-glass echoes are likely decidualized endometriomas, whereas irregular papillations, clear fluid, or enlarging solid components are more likely malignancy.
Over 11 years, our high-volume OB-GYN ultrasound unit has identified numerous decidualized endometriomas, following them through pregnancy and reassessing three months postpartum to ensure they regress to typical endometriomas. Figures 3–5 illustrate the case of a 28-year-old G1P0 at 15 weeks EGA referred for a second opinion for bilateral “complex” cysts. She reported a history of severe dysmenorrhea. The cysts had characteristics of decidualized endometriomas and subsequent scans revealed no growth. Postpartum ultrasound showed the cysts had become typical appearing endometriomas. For anyone who treats reproductive age women with endometriosis, they should be counseled that this can occur in pregnancy since most ob-gyns are unaware of this phenomenon.
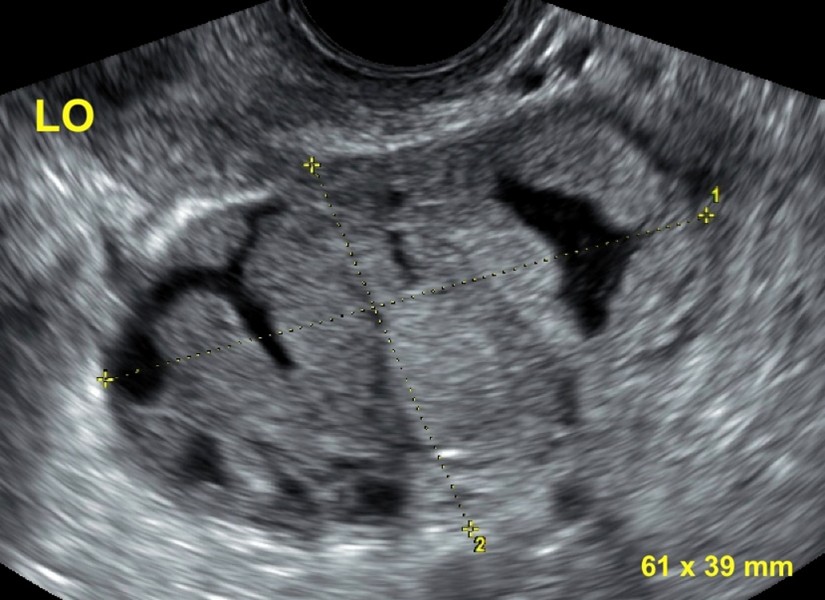 Figure 1: Sagittal image of the left ovary reveals a unilocular solid ovarian lesion. The solid components are smooth.
Figure 1: Sagittal image of the left ovary reveals a unilocular solid ovarian lesion. The solid components are smooth.
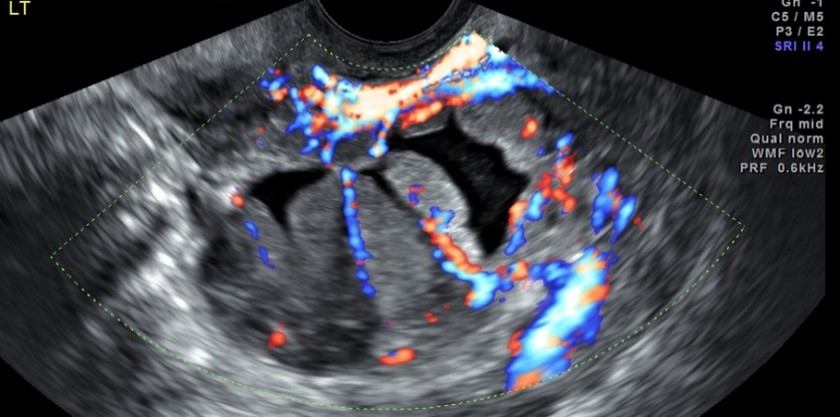 Figure 2: The solid components display moderate color flow (color score 3).
Figure 2: The solid components display moderate color flow (color score 3).
 Figure 3: Left ovary with a unilocular solid cyst, note smooth walled papillations and ground glass echoes.
Figure 3: Left ovary with a unilocular solid cyst, note smooth walled papillations and ground glass echoes.
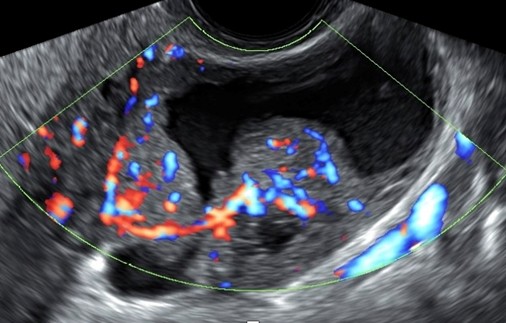 Figure 4: Abundant color flow within the papillations (color score 4).
Figure 4: Abundant color flow within the papillations (color score 4).
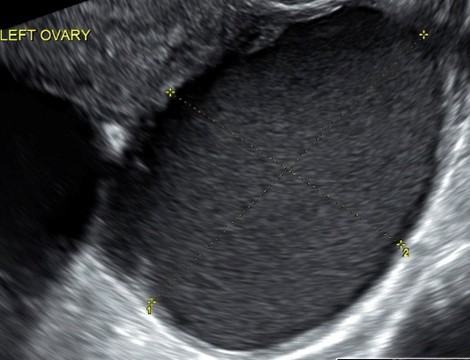 Figure 5: Three months postpartum the left ovary now contains a unilocular cyst with ground glass echoes, no papillations.
Figure 5: Three months postpartum the left ovary now contains a unilocular cyst with ground glass echoes, no papillations.
References:
- Groszmann Y., et al. Decidualized Endometrioma masquerading as Ovarian Cancer in Pregnancy. J Ultrasound Med 2014; 33(11):1909-1915.
- Mascillini F., et al. Imaging in gynecological disease (10): clinical and ultrasound characteristics of decidualized endometriomas surgically removed during pregnancy. Ultrasound Obstet Gynecol 2014; 44(3):354-360.
- Mascillini F., et al. Ovarian masses with papillary projections diagnosed and removed during pregnancy: ultrasound features and histological diagnosis. Ultrasound Obstet Gynecol 2017; 50(1): 116-123.
About the Author:
Yvette S. Groszmann, MD, MPH, FACOG, FAIUM
 Dr. Groszmann is a member of the AAGL Advanced Gynecologic Ultrasound and Imaging SIG, Director of Gynecologic Ultrasound and Diagnostic Ultrasound Associates, and a Lecturer in Obstetrics, Gynecology and Reproductive Medicine at Harvard Medical School in Boston, Massachusetts.
Dr. Groszmann is a member of the AAGL Advanced Gynecologic Ultrasound and Imaging SIG, Director of Gynecologic Ultrasound and Diagnostic Ultrasound Associates, and a Lecturer in Obstetrics, Gynecology and Reproductive Medicine at Harvard Medical School in Boston, Massachusetts.

Ultrasound in Gynecology: Embracing a Familiar Yet Underutilized Frontier
Gynecologic ultrasound is often hailed as the “workhorse” of gynecologic healthcare: accessible, non-invasive, and highly informative. Despite this, many clinicians underutilize this fundamental tool when evaluating common conditions such as fibroids, adenomyosis, or endometriosis. As a technology generally used, but not performed or interpreted by gynecologic surgeons, the door is wide open for enhanced utility, innovation, and surgical integration. Our newly formed Special Interest Group (SIG) on Advanced Gynecologic Ultrasound & Imaging aims to elevate the standard of care by blending robust foundational practices with cutting-edge innovations, including emerging machine learning (ML) applications.
Bridging Basic and Advanced Imaging
Conditions like endometriosis and adenomyosis are thought to be notoriously difficult to diagnose. While physical examination and patient history provide valuable clues, imaging is critical for precise detection and treatment planning. However, practice patterns reveal that many clinicians rely on basic, and sometimes limited, 2D ultrasound assessments—or avoid ultrasound altogether and proceed directly to MRI or diagnostic laparoscopy.
Even at a fundamental level without fancy technology, a structured approach guided by international evidence from the IDEA (International Deep Endometriosis Analysis) or MUSA (Morphological Uterine Sonographic Assessment) groups can reveal gynecologic diseases with clarity and precision (Figure 1 and Figure 2). Building on this foundation, clinicians can then employ newer modalities—such as 3D, power Doppler for vascular mapping and elastography for tissue characterization—to glean deeper insights into complex conditions. Beyond the technological advancement of ultrasound, the ultrasound academic community is pioneering understanding of pelvic anatomy like never before, with recent publications on the sonographic evaluation of the parametrium and pelvic sidewall, including sacral nerve roots. This advanced knowledge will enable us to push the envelope in diagnostics and surgical planning.
Overcoming Barriers to Adoption
One major hurdle to widespread use of gynecologic ultrasound is the perception that it is too operator-dependent or that it can’t be learned or done by gynecologic surgeons. While it is true that ultrasound’s accuracy hinges on the expertise of the clinician, structured training programs and standardized reporting can dramatically improve reproducibility. This underscores a key mission of our SIG: to provide educational resources, promote best practices, and facilitate mentorship opportunities among ultrasound users at all levels of expertise. Furthermore, new portable ultrasound systems have made the technology more accessible, enabling clinicians in diverse practice settings to perform high-quality scans with minimal investment in equipment.
Looking Ahead: Machine Learning in Endometriosis Imaging
One of the most promising frontiers in gynecologic imaging is the use of ML to assist in detecting pathologies. IMAGENDO, for example, is pioneering algorithms that analyze ultrasound scans to identify telltale signs of endometriosis. By leveraging large datasets, these systems can detect image patterns, potentially hastening the diagnosis of a disease that historically has taken years to confirm. ML-driven tools offer a new level of diagnostic support, suggesting potential areas of pathology in real time and providing quantitative risk assessments. While these methods are still emerging, early data point to increased accuracy and a promising avenue for reducing diagnostic delays.
A Collective Vision for Better Care
The Advanced Gynecologic Ultrasound & Imaging SIG was formed with a clear objective: to empower gynecologists to use ultrasound as a first-line, highly effective diagnostic tool, while simultaneously exploring the frontiers of new imaging technologies. By focusing on both foundational skills and state-of-the-art innovations, we aim to elevate clinical practice, foster collaboration, and, most importantly, improve patient care.
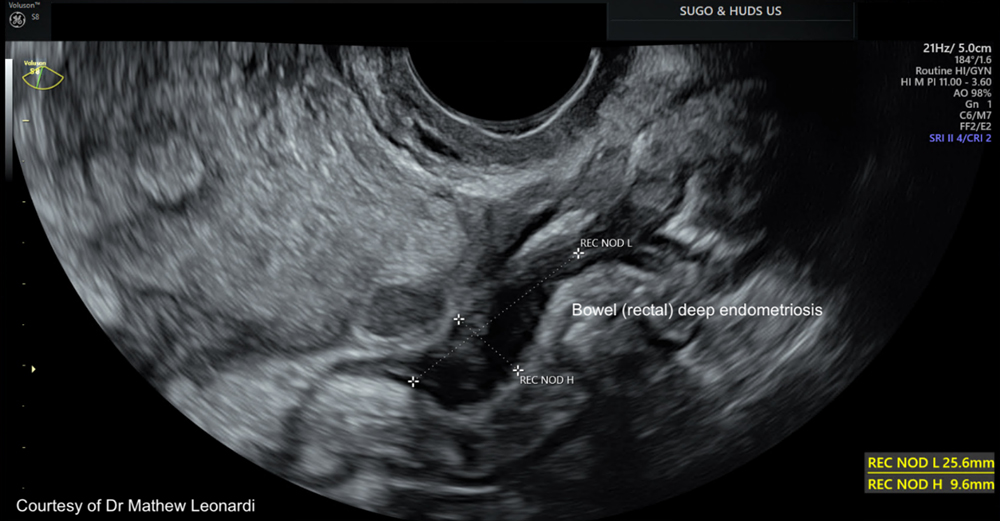 Figure 1: Rectal endometriosis
Figure 1: Rectal endometriosis
 Figure 2: Features of adenomyosis
Figure 2: Features of adenomyosis
About the Author:
Mathew Leonardi, MD, PhD, FRCSC

Dr. Leonardi is a member of the AAGL Advanced Gynecologic Ultrasound and Imaging SIG, a Surgeon Sonologist at Hamilton Health Sciences, Assistant Professor at McMaster University, and Director at Specialized Ultrasound in Gynecology & Obstetrics in Hamilton, Canada