Doctors Most Challenging Case: Trials and Tribulations of Ovarian Transposition for Women with Cervical Cancer

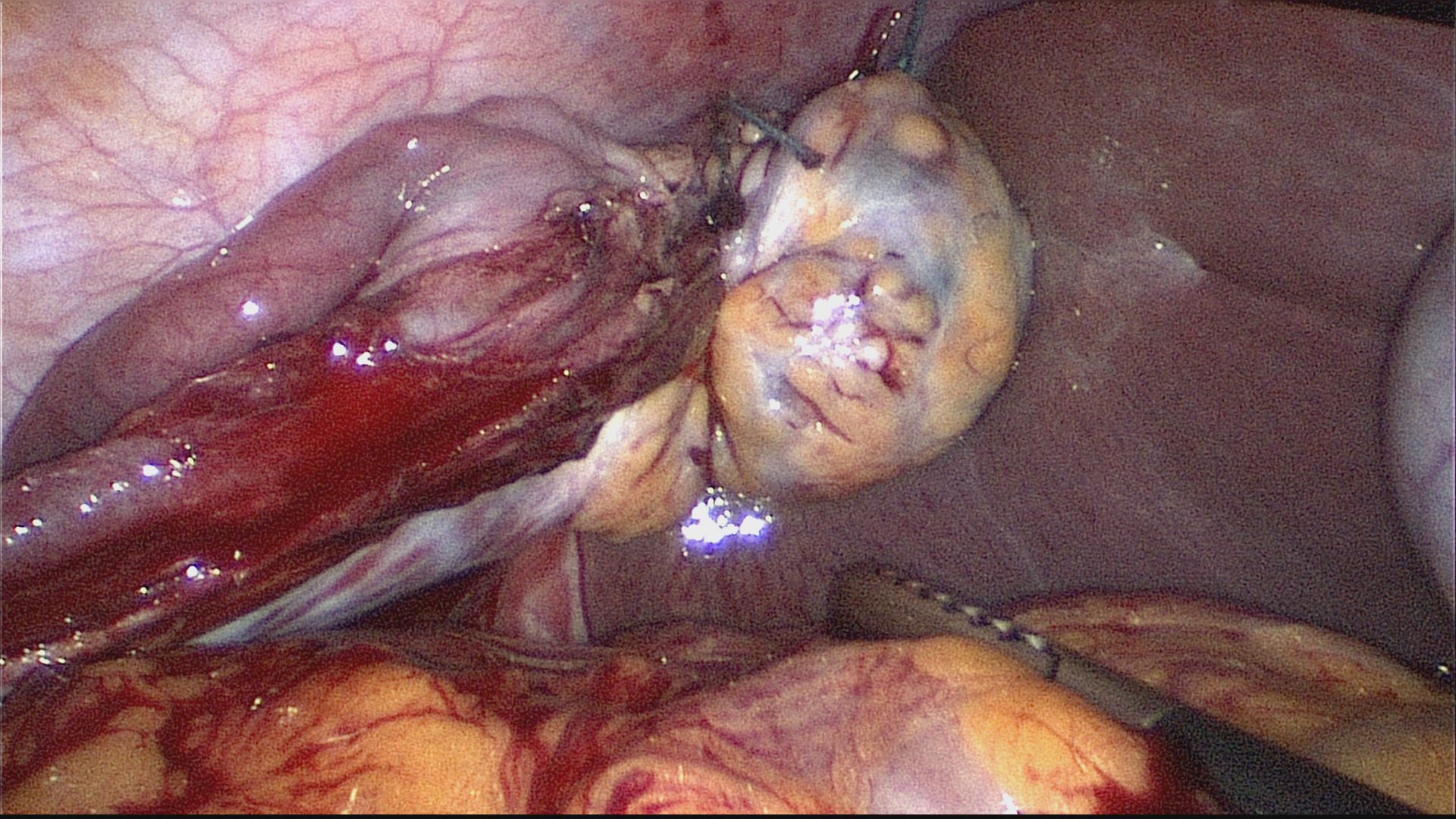
In the past months we have featured cases and articles from AAGL’s Robotics, Hysteroscopy and Pelvic Pain – Special Interest Groups (SIGs) and in this issue, the Oncology SIG takes the spotlight! The most difficult case has to deal with ovarian transposition for women with cervical cancer, pictured in the image below.
Thanks to all the AAGL SIG chairs, vice-chairs and members – for the informative and timely articles and for supporting this exciting series! If you would like to join an AAGL SIG in Urogynecology, Robotics, Oncology, Endometriosis, Pelvic Pain or Hysteroscopy, contact Seth Spirrison via email to sspirrison@aagl.org. Your AAGL membership must be current and in good standing.
A 32-year-old healthy woman was diagnosed with an HPV-16 associated stage IB3 adenocarcinoma of the cervix a year following vaginal delivery of her first child. She desired ovarian transposition (OT) in advance of primary radiation (RT) with radiosensitizing cisplatin. Laparoscopic transposition of the right ovary anterolaterally along the right costal margin (see image) was uneventful. An enlarged pelvic lymph node (PLN) was uncovered during exploration of the left pelvic sidewall prior to left OT. Left OT was abandoned despite negative frozen section histology of the enlarged left PLN. Final histopathologic evaluation of the left PLN revealed an isolated 2mm micrometastasis.
As assisted reproductive technologies have evolved, delayed childbearing has become more common and large epidemiologic studies have raised awareness of the long-term health risks of premature ovarian insufficiency (POI). Preservation of ovarian function has become an important part of the discussion prior to cancer treatment for many women. This is particularly true for cervical cancer (CC), as over a third of US women are ≤ 45 yo at diagnosis and often face treatment with pelvic radiation. OT is the sole means for protecting the ovaries from gonadocidal doses of radiation by surgically relocating them outside of the radiation field. A recent review of the 2009-2016 MarketScan database suggested that less than 10% of women ≤ 35 yo undergo OT prior to pelvic RT for newly diagnosed CC. Underutilization appears to be related to gaps in fertility preservation knowledge, concerns about oncologic safety and lack of availability of surgeons proficient at performing the procedure [1]. However, as ovarian preservation is increasingly valued among patients and providers, guidelines for OT that take into account our current understanding of the oncologic safety, practice and effectiveness of OT are needed. For women with CC, these should include the following key considerations:
- Risk of occult ovarian metastasis is highest in cases of bulky tumors (≥ 3 cm), ≥ stage IIB disease, adeno/adenosquamous histology and lymphovascular invasion. In these cases, the oncologic safety of OT should be carefully weighed [2].
- PLN involvement occurs with 9-30% of stage IB and 7-50% of stage IIA CC. Available data indicate that para-aortic LN involvement is rare when PLN micrometastases (≤ 2mm) are present [3,4]. Whether the risk of occult ovarian metastasis is similarly low in the setting of PLN micrometastasis is uncertain.
- A personal or family history suggestive of a hereditary ovarian cancer syndrome is a relative contraindication to OT.
- There is no consensus concerning the location of transposed ovaries, although the general agreement appears to be as high and as lateral as possible away from the pelvic RT field. The approach to transpose ovaries to a high anterolateral position at least 3-4 cm above the umbilical line (as opposed to aiming for5 cm above the iliac crest in the paracolic gutter) has merit in the event an extended radiation field is indicated [4]. Whether concomitant opportunistic salpingectomy (removal of the fallopian tubes for the primary prevention of ovarian cancer at the time of pelvic surgery) is inadvisable due to a compromise in ovarian blood flow that negatively impacts ovarian function remains unknown.
- Intraoperative frozen section evaluation of LNs has limited diagnostic value due to failure to detect micrometastasis and small macrometastases. The false negative rate is 8-32% and depends on the intraoperative frozen section protocol used, for which there is no current standard [5].
- Ovarian/fertility preserving procedures can delay cancer care. Surgical staging for CC has been associated with a median 2 week delay in initiation of radiation [6]. A 2 week maximum delay following OT should be the goal.
- The OT literature indicates that ovarian function is effectively preserved in 50-70% of CC patients following pelvic RT. Age above 40 years has often been used as a cutoff point. However, more recent data indicate that durable ovarian function is much lower among women age 35-40 yo [7]. Thus, the more limited chances of long-term ovarian survival following OT for women ≥ 35 yo should be factored in their individualized risk-benefit assessment.
- Young women who experience POI due to gonadotoxic therapy should be considered for and counseled about hormone replacement therapy (HRT). While limited retrospective data indicate that HRT may insufficiently replace the benefits of native ovarian function, more conclusive evidence is needed [2,4].
[1] Selter J, Grossman Becht LC, Huang Y, Ananth CV, Neugut AI, Hershman DL, Wright JD. Utilization of ovarian transposition for fertility preservation among young women with pelvic malignancies who undergo radiotherapy. Am J Obstet Gynecol. 2018;219(4):415-417.
[2] Yamamoto R, Okamoto K, Yukiharu T, Kaneuchi M, Negishi H, Sakuragi N, Fujimoto S. A study of risk factors for ovarian metastases in stage IB-IIIB cervical carcinoma and analysis of ovarian function after a transposition. Gynecol Oncol. 2001 Aug;82(2):312-6.
[3] Nica A, Gien LT, Ferguson SE, Covens A. Does small volume metastatic lymph node disease affect long-term prognosis in early cervical cancer? Int J Gynecol Cancer. 2020 Mar;30(3):285-290.
[4] Hwang JH, Yoo HJ, Park SH, Lim MC, Seo SS, Kang S, Kim JY, Park SY. Association between the location of transposed ovary and ovarian function in patients with uterine cervical cancer treated with (postoperative or primary) pelvic radiotherapy. Fertil Steril. 2012 Jun;97(6):1387-93.
[5] Scholz HS, Lax SF, Benedicic C, Tamussino K, Winter R. Accuracy of frozen section examination of pelvic lymph nodes in patients with FIGO stage IB1 and IIB cervical cancer. Gynecol Oncol. 2003 Sep;90(3):605-9.
[6] Yang J, Delara R, Magrina J, Magtibay P, Yi J, Langstraat C, Robertson M, Dinh T, Butler K. Comparing survival outcomes between surgical and radiographic lymph node assessment in locally advanced cervical cancer: A propensity score-matched analysis. Gynecol Oncol. 2020 Feb;156(2):320-327.
[7] Hoekman EJ, Knoester D, Peters A, Jansen FW, de Kroon CD, Hilders C. Ovarian survival after pelvic radiation: transposition until the age of 35 years. Arch Gynecol Obstet. 2018 Nov;298(5):1001-100eated perforation in the uterine wall.